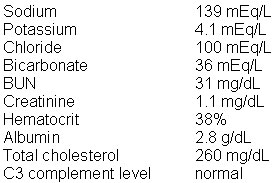
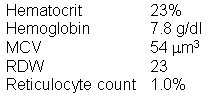
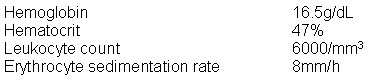
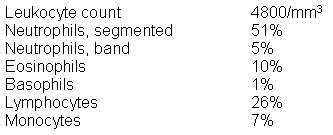
An 8-year-old boy is brought to the office by his mother because of recurrent episodes of "shortness of breath" and wheezing. These episodes typically occur when he is playing in the park with friends or when he is in the house at night. The symptoms are worst in the springtime and when he is watching television with his mother's boyfriend. The mother's boyfriend, who happens to smoke cigarettes, has been spending more and more time at the house, trying to bond with the patient. Pulmonary function tests show that the peak expiratory flow and forced respiratory volume per second are reduced during an attack and are normal during symptom-free intervals. Skin testing shows that he is allergic to grass and tree pollen, dust mites, animal dander, and a variety of other allergens. Laboratory studies show:
The most appropriate next step is to
| Explanation: The correct answer is C. This patient has asthma, and the most crucial step in the management of asthma is avoidance of the triggering factors, e.g., allergens. Unfortunately, it is difficult to avoid specific types of allergens, such as pollens. Specific measures to eliminate or reduce exposure to dust mites and animal dander at home lead to a reduced frequency of attacks and hospitalization rates. Regardless of the allergens involved, elimination of respiratory irritants, especially cigarette smoke, is of crucial importance. The bronchial tree of asthmatic patients is highly reactive to any form of chemical or physical irritation. Thus the avoidance of passive smoke is important. The mother should ask her boyfriend to go smoke outside alone if he needs to, but he should not be allowed to smoke in the house. It is not practical to administer immunotherapy against identified allergens (choice A) in this case because he is allergic to multiple airborne allergens, and it seems like he is especially responsive to cigarette smoke. Immunotherapy is of some benefit when a single allergen is identified. The most important step is to try to reduce exposure to avoidable allergens (smoke). Avoidance of all exercise (choice B) is not appropriate because even though exercise triggers asthmatic attacks in some patients, this does not seem to be his main trigger. Humidifiers and air cleaners (choice D) at home is not the appropriate management. Humidifiers favor the growth of dust mites, and air cleaners have not been shown to be uniformly effective in getting rid of dust mites. It is inappropriate to prescribe inhaled sodium cromoglycate, oral corticosteroids, and oral theophylline (choice E) for this patient because the fewest number of drugs at the lowest effective doses should be used. Typically, a one drug regimen (a bronchodilator or an inhaled corticosteroid) for mild to moderate asthma or two drugs for more severe cases is sufficient to control asthma exacerbations. Oral corticosteroids are indicated in cases of severe asthma and are therefore, not for this patient. |