| Explanation: The correct answer is B.
This patient most likely has Pneumocystis carinii
pneumonia (PCP), and she is probably infected with the human immunodeficiency
virus (HIV), in her case, most likely due to unprotected sexual intercourse
with an infected individual. It is important to recognize that elderly patients
may be sexually active, even if their spouse is no longer around. They are
at risk for HIV and other sexually transmitted diseases because they may not
think to use a condom because they are not worried about getting pregnant.
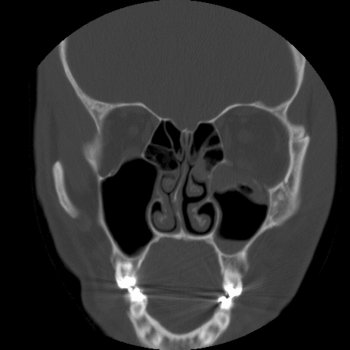
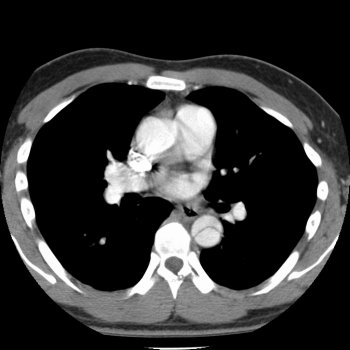
PCP is characterized dyspnea, fever, a nonproductive cough, retrosternal
chest pain, tachypnea, tachycardia, few abnormalities on auscultation, bilateral
patchy alveolar infiltrates on chest x-ray, and round cysts found under light
microscopy when stained with methenamine silver. The treatment is trimethoprim-sulfamethoxazole.
The "episode of fever, headaches, joint pain, a loss of appetite, and mild
sore throat" that she describes having a few months earlier is consistent
with the acute HIV syndrome which affects many patients with HIV, approximately
three to six weeks after the primary infection. This syndrome coincides
with plasma viremia (wide dissemination of the virus). The symptoms gradually
subside over a few weeks. "Did you or your late husband ever install insulation or brake lining,
do construction work, or work in a shipyard?" (choice A) is an important question if an asbestos-related disease
is suspected, but this case is more consistent with Pneumocystis
carinii pneumonia than asbestosis
or malignant mesothelioma. Asbestosis is characterized by dyspnea, a nonproductive
cough, basilar crackles or rales, clubbing, linear streaking and pleural thickening
seen on chest x-ray, and ferruginous bodies seen on microscopic examination
of lung tissue (rod-shaped bodies with clubbed ends). Malignant mesothelioma
is a tumor of the pleura that is characterized by chest pain, dyspnea, a cough,
a chest x-ray showing pleural fluid, irregular pleural thickening, and a biopsy
demonstrating the malignant cells. "Have you ever been involved in a homosexual relationship?" (choice C) is not a vital question at this
time because it is very unlikely that this woman contracted HIV and AIDS from
unprotected sexual intercourse with another woman. It is more likely that
she contracted the infection from unprotected sexual intercourse with a man.
Also, if you wanted to know if a patient has homosexual relationships, it
is better to ask in a nonjudgmental way, such as, "Do you have sex with men,
women, or both?" "Have you ever had drink in the morning to get started (an "Eyeopener")?" (choice D) is a part of a four question screening test to detect problem
drinking called the CAGE questionnaire. The other three questions that make
up the CAGE questionnaire include: “Have you ever felt the need to Cut
down on your drinking?”, “Have you ever felt Annoyed by criticisms
of your drinking?”, and “Have you ever had Guilty feelings about
drinking?”. Two positive responses indicate that a problem is likely.
These questions may be important, but the immediate concern in
this case is this patient's Pneumocystis carinii pneumonia and whether she has been infected
with the HIV virus. Questions related to her sexual practices may help to
identify the source of infection. "Have you ever had a positive PPD or been exposed to anyone with tuberculosis?" (choice E) is a question that is important if tuberculosis or an aspergilloma
is suspected. However, this case is more consistent with Pneumocystis carinii pneumonia.
Primary tuberculosis (TB) is characterized by systemic symptoms, a cough,
sputum production, hemoptysis, lower lobe infiltrates, hilar node enlargement,
pleural involvement, and the presence of acid-fast bacilli. Reactivation
TB is characterized by infiltrates with cavitation in the apices. An aspergilloma
is a "fungus ball"' that typically forms within a preexisting cavity (from
TB or sarcoidosis) in the pulmonary parenchyma. The patients may be asymptomatic
or present with hemoptysis. A culture shows fungal mycelia, which appear
as branching hyphae. In this case, microscopic evaluation shows round structures,
not acid-fast bacilli or hyphae. |